Partial ACL tear
Isolated ruptures of the anterior cruciate ligament (ACL) injuries are the most frequent ligament of the knee. These breaks may be complete or partial. In partial tears, clinical diagnosis is more difficult because the clinical presentation is variable.
Diagnosis, time course, and treatment its partial tears are still subject to much controversy. The purpose of this article is to clarify the definitions, clinical diagnosis and therapeutic strategies to these partial ACL tears.
Anatomy and biomechanical ACL
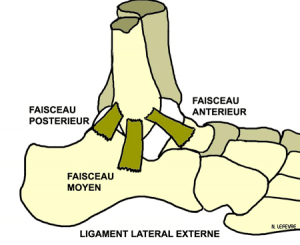
The LCA has two main beams: the anteromedial bundle (AM) and posterolateral bundle (PL).
Biomechanically, the AM beam, more isometric, allows control of the anterior tibial translation in the femur, the knee flexed. He participates in the control of internal and external rotations. The posterolateral beam, thicker, less isometric, it is more specifically devoted to the control of anterior translation, hyperextension and rotations. Its oblique position allows him a better control of rotations.
The AM is taut in flexion (PL is then relaxed).
The PL is taut in extension and internal rotation.
The position of the knee at the time of trauma might explain a preferred lesion of one of the two beams. Theoretically, a rupture of the AM bundle should lead to laxity in flexion, to stable knee extended and the absence of clinical rotation anomaly. Similarly, the isolated tear PL beam should theoretically result in anterior laxity in extension, an increase in internal and external rotation in extension. This, at least, what happens in sequential sections ACL cadaver lab.
Moreover, before experiencing a break, the fibers can lie approximately 50% (plastic deformation) or cause interstitial break with a macroscopic appearance nickname intact fibers (with distension difficult to appreciate), but a fiber continuity between the tibial and femoral insertion sites.
The healing capacity of the ACL after trauma is relatively limited but possible, given the precarious ligament vasculature.
Ischemic necrosis of residual fibers of the ACL is therefore possible by insufficient vascularization explaining the transition from partial rupture to complete rupture. This insufficient healing associated to microscopic damage to the ligament structure defines the functional incompetence ACL traumatized. Clinically, this will lead to recurrent instability of the knee.
Definition of a partial ACL tear
A partial disruption should cover a ligament injury grade 2, that is to say, a distension without interrupting the continuity of the fibers. A partial rupture can match
- either a simple MRI bleeding at the point of insertion of femoral ligament
- either a ligament aspect distended, but continuous MRI or arthroscopy
- either a complete break isolated from either AM or PL beams …
The percentage of broken fibers may also be the criterion with partial lesions of interest from 25 to 75% of the fibers or a subdivision in high grade (> 50%) or low grade (<50%).
Finally, if the rupture often interested femoral insertion, interstitial breaks can be considered as partial tears ( “continuity”).
The diagnosis of a partial tear is based on the combination of:
- low patient’s sensation of instability or absent
- asymmetric laxity in low Lachman test, usually with a hard stop
- lack of pivot shift or rotational jump. (isolated AM bundle)
- a differential laxity at TELOS review or weak GNRB
and 5th criteria: appearance ACL MRI 3D CUBE
when these 4 criteria are used, the diagnosis is based on the laxity and not on the residual structure of the LCA (MRI CUBE), but it confirms the diagnosis
- If These four criteria are met, the patient is diagnosed carrying a partial tear and ACL (residual) is considered a priori functional.
- Si Structural lesions are sufficient to cause a positive pivot shift, then the LCA (residual) is considered non-functional. The pivot shift test therefore would distinguish partial tears with residual functional and non-functional ligament.
Laximetry objective: TELOS GNRB
The testing by TELOS or GNRB can be discriminant to distinguish partial rupture and complete rupture. Thus, some patients with a positive pivot shift can have a laximétrique differential of less than 3 mm. Quantitative measurement by laximetry is an interesting complement to the evaluation of the anterior laxity of the knee.
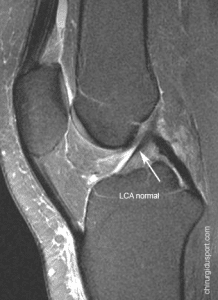
MRI Cube
Some MRI images suggest the existence of a partial tear, but can not firmly establish the diagnosis. The criteria usually retained to evoke a partial rupture are:
- a signal intensity within the LCA;
- a relaxed or thinned appearance or wave ACL, but with fiber continuity of the femur to the tibia
- a respected overall orientation.
The standard orthogonal slices do not analyze well the oblique structure. Additional oblique cuts can be usefully added. The value of MRI is useful CUBEto better identify the two beams.
More than half of the partial tears can not be differentiated solely on complete rupture MRI data. The sensitivity of this review would be 55% with a specificity of 75% in their detection.
arthroscopy
Because the clinical evaluation of these partial tears is difficult, many authors use arthroscopy during surgery as reference examination to define the extent of the fracture. The assessment is however not easy because of the following
- An apparently intact tissue may have interstitial lesions;
- The residual tissue may have undergone plastic deformation (expansion);
- Synovial environment can be preserved, but the fibers are, they traumatized;
- Rupture often interested in the femoral insertion of the ACL and the foot may appear normal;
- A complete break can heal in the notch or rather firmly LCP giving an aspect of ligament “vertical”, but tense.
The evaluation of the quantity and quality of residual ACL is not so easy in arthroscopy. Some authors found a correlation between the clinical findings and the amount of residual ACL observed in arthroscopy, some not …
Treatment
The treatment of patients with these partial lesions must be fixed and must take into account the patient’s symptoms (feeling of instability), physical examination of the data, the amount of residual ligament, sport, the sporting, the time intervals from the initial trauma, work requirements …
Functional treatment may be reserved for patients in whom few applicants sports application is limited and the risk of developing a functionally unstable knee (positive pivot shift) less pronounced. In sportier patients, the risk must be explained and surgical treatment considered especially if a pivot shift appears.
Conservative treatment
Conservative treatment is variable combining the use of splint, rehabilitation, muscle building. The healing period is three months.
Wearing a splint has not proven its effectiveness in the prevention of progression to a complete break with the resumption of sporting activities. If instability is revealed, it is then necessary to move towards a ACL reconstruction processing.
Surgical treatment
The first complete stock by performing testing under general anesthesia.
For some authors, the sensitivity of the pivot shift would be 24% of the patient awake and 92% on the patient under general anesthesia. This is, for them, the major diagnostic criteria.
- If The pivot shift under anesthesia is negative, a diagnostic arthroscopy is performed to remove a meniscal tear, osteochondral or a stump associated LCA.
Treatment can be either a complete ligament, partial ligament or very rarely a drug therapy based on the appearance of the scar LCA
- If The positive pivot shift is under general anesthesia, surgery is performed.
The single beam reconstructions
Repair (suture) the broken beam can be considered, but few results related to it. Selective reconstruction beam (AM / PL) damaged (increase) is the proposed treatment when surgical decision is made.
Back to Sports
Patients with complete healing of the ACL can take a full sport at the same level.
But certain patients treated functionally may have a decrease in the intensity of their sport and are moving towards less restrictive sports for the knee. The function and stability are acceptable under these conditions limiting rotation activities.
associated lesions
Partial tears may be associated with meniscal lesions (medial> lateral) or cartilage. This does not influence in the literature, the clinical results or the need for recourse to reconstruction surgery.
Risk of further joint degeneration
There is little data in the literature and series are too few to assess the fate of these knees.
But we believe that if the knee is stable, secondary osteoarthritis risk is not greater knee operated or not
Conclusion
Clinical examination is fundamental for the detection of partial lesions. A partial tear of the anterior cruciate ligament (ACL) is characterized by an asymmetric laxity in the Lachman test, a test of negative pivot shift and a differential laxity measured by test TELOS GNRB weak, all associated with arthroscopic aspect of ACL injury .
If a partial rupture is suspected, the approach must focus on functional quantification of residual ACL. Structural analysis (IRM) can not be sufficient and decisive to guide therapeutic choices.
Other clinical tests, laximétrique measurement and MRI lesion can estimate the degree.
Functional treatment gives acceptable results in the majority of cases.
The progress of the laxity (anterior drawer in rotation) will depend on the size of the ACL injury.
Symptomatic instability is treated by surgical reconstruction of the ACL.
The subject of partial tears of the anterior cruciate ligament (ACL) is booming and interest on the rise for several reasons:
- The anatomy of the ACL, including arthroscopic, having been rediscovered at the development of ACL reconstruction techniques dual beam, analyzing residual fiber ACL is now thinner.
- The laxity are often operated at an earlier stage that a few years and the number of knee where there is ligamentous structures, albeit incomplete, is steadily increasing in our daily practice.
- Functional medical treatment, often used, is known for its results entirely acceptable but showed, despite all its limitations regarding the return beforehand athletics.
- Imaging techniques, including MRI cube, progress and allow radiologists to suspect these incomplete without breaks, however, able to fully characterize.
Doctor Nicolas LEFEVRE, Doctor Yoann BOHU, Doctor Antoine GEROMETTA, Doctor Serge HERMAN. – 15 novembre 2015.