indications
The shoulder dislocations and recurrent anterior instability is a common problem among young athletes making up 90% of shoulder dislocations. Surgical indication can be provided in these cases of glenohumeral dislocations previous recurrent, but also in cases of painful and unstable shoulders. A question now arises, should we offer it immediately after the first dislocation or should we expect one or more recurrences?
The current trend as found in the literature would suggest surgery earlier or even after a first dislocation in some cases. This should depend on several factors: young age, sport practiced at risk or competition (armed or armed-countered: handball, volleyball, basketball), the hyperlaxtié and loss of initial substances glenoid bone and humeral objectified on the preoperative scanner.
Indeed, in these at-risk patients, the recurrence rate is high and complications of chronic instability can occur.
Stabilization techniques
Today there are 2 stabilization techniques:
- The coracoid bone block screwed in front of the glenoid realized today either open or arthroscopically.
- The rehabilitation of the anterior rim and retry capsuloligamentous by Bankart. However, the mere rehabilitation labral and capsular retention may not be sufficient in patients with poor quality tissue or bone defects.Indeed this technique reported lower results than in the presence of glenoid or humeral bone defects type lesions Hill-Sachs.
In case of failure or in the presence of Bankart lesions mentioned above, the Latarjet arthroscopic or open procedure is a reliable and durable method for the treatment of anterior instability with long-term satisfactory results. Nowadays, this intervention is entirely feasible under arthroscopy. This technique described by Laurent Lafosse started in 2005 and is gradually developing in France and abroad with growing interest.
The advantages of arthroscopic technique are:
- Take stock of the damage to the joint, bead, cartilage, loss of bone substance, tendon injuries
- Propose an anatomical repair Arthroscopic Bankart kind if this is justified
- The precise positioning of the stop because under direct control by the camera,
- Of smaller sizes scars,
- The treatment of lesions as lesions of the biceps (SLAP lesion) or lesions of the rotator cuff (tendon rupture) that can be treated in the same operation
- Early functional recovery
The steps of surgery are similar to that carried out in the open. It is, however, a technically demanding procedure that has a relatively long learning curve.
Latarjet arthroscopic intervention
The procedure is most often performed under general anesthesia with an inter-scalene block made ??preoperatively by the anesthetist. It involves taking a bone block of about 2 cm at the expense of the coracoid and place it in the anterior and inferior part of the glenoid cavity, passing through the subscapularis muscle. The coracoid can be positioned upright and secured by a screw according to Bristow or lying and fixed by two screws according Latarjet.
Stabilization through the stop effect produced by the bone block, the hammock effect created by the tensioning of coracoacromial biceps inserted on the tip of the coracoid.
It is a demanding process, but with a reliable and reproducible technique.
surgical Technique
The technique has 10 surgical steps. The patient is in a semi-sitting position.
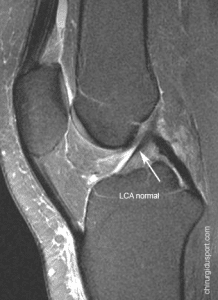
Step One: Assessment of the articulation
The most important anatomical landmarks (acromion, clavicle, coracoid, the tendon of the subscapularis), the first track and the axis of the joint are previously carried on the skin. (Figure 1) Then the joint is assessed by the posterior optical path (A). This includes assessment of dynamic stability, deformities and glenoid and humeral anomalies, as well as HAGL lesions. The description of the procedure is validated after the evaluation. The advantage compared to the open procedure Latarjet is to be able to offer this time after anatomic repair Arthroscopic Bankart kind if this is justified as well as being able to treat concomitant lesions like SLAP or lesions of the posterior labrum.
Second Step: Preparation of the joint
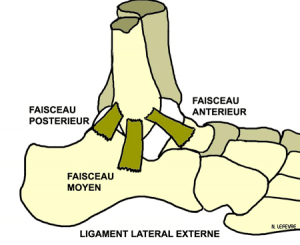
The anterior rim and the cap are removed from 2 to 5 hours, and the average glenohumeral ligament and the anterior portion of the glenohumeral ligament lower through first (E) until the muscle fibers subscapularis are exposed. We must make 2 marks on the glenoid rim at 2 and 5 hours will be the upper and lower marks for precise positioning of the coracoid process to the end of the procedure.
Third step: preparing coracoid
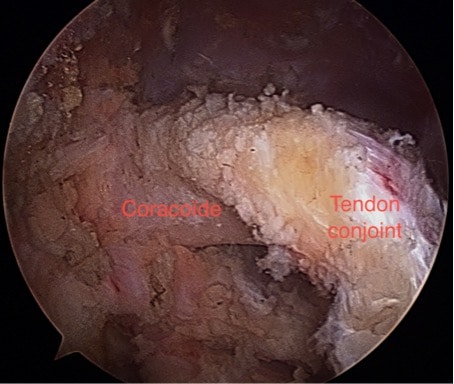
The path (D) anterolateral is now created.The coracoacromial ligament is detached from the coracoid and must release the side of the joint tendon deltopectoral fascia. Care must be taken not to damage the joint tendon.
The arthroscope is then moved in the direction (D), which creates ways (I) and (J) under direct vision using two hands to lumbar puncture. The medial path (M) is created using a switching-stick from behind by the channel a to be in the plane of the coil, at the lower glenoid mark.Then, with the arthroscope through (I) opposite the tip of the coracoid, the medial part of the coracoid process is accessible and detachment of the pectoralis minor is made. A switching-stick is placed through (D) to lift the deltoid creating a workspace. the medial joint is released tendon soft tissue taking care of the superficial peroneal nerve.
The upper face of the coracoid process is prepared to the base which is defined by the coracoclavicular ligaments.
Step four: Charge of the coracoid
The path (H) is created to accommodate the coracoid drill guide.The tip of the coracoid is identified by a pin to properly position the guide.
Two pins of 1.5 mm are inserted using the guide, about 5 mm from the tip of the coracoid and between average and medial third of the process (2/3 and 1/3 medial side). Once the pins are inserted, the guide is removed and the position confirmed with arthroscopy in the way (I). Holes are then drilled and tapped. A washer is then inserted into each hole by using the spindle as a guide. The next stage is the circumferential weakening of the base of the coracoid process using a cutter.This is done by different ways, by means (M) (2-6h), through (D) (6-11h) and the upper part through (H) (11-2h) bearing in a spindle the proximal hole as a benchmark for the lower milling. After resection of cortical bone at the base of the coracoid made ??circumferentially, the osteotomy is performed from the channel (H) with a bone chisel curve. The coracoid is mobilized medially to expose entirely the anterior surface of the subscapularis.

Step Five: The preparation of the subscapularis split
The previous award of the subscapularis is removed with a shaver to view all of the subscapularis muscle, including the “three sisters” (anterior circumflex humeral artery and two veins), marking the lower limit.Using the arthroscope through (J) and the probe electrocoagulation through (M), the split is made ??at the lower 1/3 of the muscle. It is critical during this step to free enough laterally to the insertion on the lesser tuberosity and within, using external and internal rotation to expose the muscle and the tendon. The axillary nerve defines the medial limit of the split. The switching -Stick of the posterior approach (A) is used to lift the upper portion of the tendon through the split and open space.
Step Six: The exhibition and preparation of the glenoid
The glenoid bone surface is now prepared by keeping scope through (I) and the instruments through (E). The use of electrocautery then the cutter will allow to obtain a spongy bone surface bleeding to be planar.
Step Seven: Recovery of the coracoid
The path (M) is now expanded and the trocar is inserted to split the pectoralis major. The double cannula with those blue introducers is introduced via the route (M). The two introducers are removed together and long mounting screws 3.5 mm are used to engage and secure the coracoid to the double cannula. the coracoid is mobilized, this allows you to remove the remaining soft tissue on the medial side and facilitating the mobilization.The underside of the coracoid process, which will be in contact with the glenoid cavity, is sharpened and flattened to the base to position easily. The assistant holds the arthroscope in the gate (I) while the surgeon mobilizes the graft with the double cannula for better control milling.
Eighth step: Placement of the coracoid
In order to place the graft parallel to the plane of the glenoid and therefore ensure that it is not overwhelming, it is useful to retract the scapula. The arm is then placed in internal rotation and a slight bending forward so as to relax the joint and tendon of the subscapularis split open, thus facilitating proper placement of the graft. The double cannula is then used to manipulate and position the graft to the glenoid through the split of the subscapularis. The switching-stick to the path (A) is used to open the split allowing the passage of the graft. The switching-stick is also used to check the positioning of the graft, to prevent graft overflowing from the glenoid . The optimal positioning is about 1-2 mm medial to the cartilage surface. The graft will be placed between pins initially prepared (2-5h), the lower guide pin is inserted through the long cannulated screw: it is only inserted about 2 mm to ensure a bone contact but that can still turn around thereof for the optimal placement of the graft. Once the correct position is obtained, the two pins are introduced, starting from the top and then placing the lower spindle, via the cannula through the graft and the glenoid cavity until they perforate the skin back. The pins are held firmly by clamps back to ensure that they remain in place during the drilling and fixing of the graft. Looking at the shoulder by a top view, the two pins back must deviate from the switching-stick (alpha angle) of about 10 degrees. They should be parallel to avoid divergent screws.
Step Nine: Fixing the coracoid
The lower hole is drilled first to ensure good positioning of the screw in the bone. The cannulated screw (alpha) is removed and the hole is drilled by a cannulated drill of 3.2 mm. Measuring the length of the screw is made ??directly by reading on the wick to the crossing of the posterior cortex of the glenoid (usually 34-36 mm). The lower screw is then inserted and the process is repeated for the other screw.The screws are then tightened alternately to ensure symmetrical compression of the graft to the glenoid.

Tenth and final step: Joint Evaluation
The position of the graft is performed by channels earlier (I) and posterior (A). It is ideally located between 2 and 5 hours. The Kirschner wires are then removed back before removing the cannula forward.
Finally, the positioning of the graft is checked. The anti-dislocation effect can be immediately visible with the arm in abduction and external rotation. The way (J) is used to check the positioning of the graft from another point of view and get a 3D perspective; the screws must be away from the humeral head to avoid conflict.
Conclusion:
The arthroscopic procedure Latarjet is safe, reliable and reproducible in the hands of experienced and qualified surgeons. This technique, however, is changing with changing some steps and improved instrumentation.
Doctor Antoine GEROMETTA, Doctor Yoann BOHU, Doctor Nicolas LEFEVRE. – 25 octobre 2015.