Introduction
Achieving the hamstrings are the most common muscle injuries in athletes. She is well known sports physicians, coaches and athletes. contact sports, running and jumping are the most commonly involved [1-6]. Football and rugby modern are responsible for a large number of muscle injuries. Depending on the series from 12 to 16% of injuries in football and 18 to 23% of injuries in rugby cause muscle damage hamstring [1,5,7]
However, the high and complete rupture of the hamstring tendons, tendon avulsion, at the ischial is rare. The severity of the injury is often underestimated. There is no consensus on treatment. Functional treatment of these lesions simply by immobilization in a splint flexion knee gives bad results, unlike the early surgical treatment and / or late.
The objective of this study is to present our experience and results on the treatment of this rare lesion.

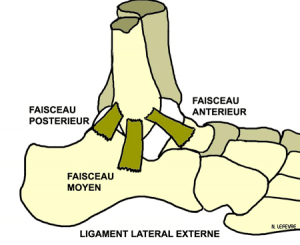
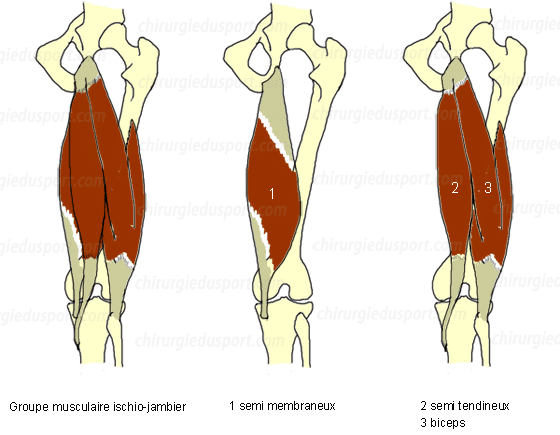
Anatomy :
The hamstring muscle group consists of three muscles of the posterior region of the thigh:
- the biceps femoris muscle (long head)
- the semitendinosus muscle and
- the semimembranosus muscle.
They are mainly flexors and secondarily leg extensors of the thigh. When walking or running, they are also antagonists quadriceps, slowing the advance of the leg at the end of the step and preventing the brutal and full knee extension.
They fit up on the ischial tuberosity and down on the tibia (Bridle) and the head of the fibula. (Figures 1 and 2)
The long head of the biceps femoris and semitendinosus have a common tendon on the posteromedial part of the ischial tuberosity. The semimembranous has isolated a large tendon that inserts into the ischial tuberosity outside the common tendon and the long head of biceps tendon semi. Behind this muscle group travels the sciatic nerve.
Material and method :
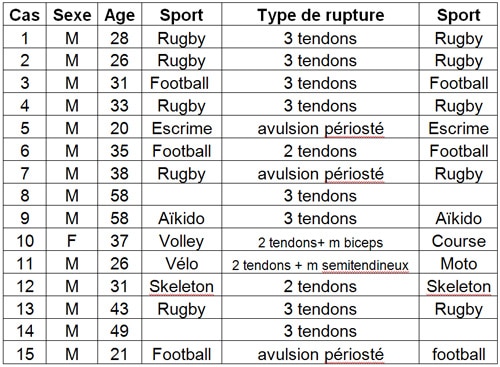
Between 2002 and 2008, 15 patients underwent a complete or partial rupture of the upper part of the hamstring tendons (Table 1). Thirteen patients were operated in emergency and 2 late after 2-3 months. There were 13 athletes and 2 sedentary. It was 5 rugby accident, 3 football accident, a case of fencing, an aikido accident, a bicycle fall, a skeleton accident, a case of volleyball, and 2 domestic accidents (falls ). We operated 14 men and one woman, average age of 35.1 years (20 to 59).
The traumatic mechanism was of two types:
- A straight leg brutal hip flexion (forward drop foot fixed to the ground).
- A brutal extension of the hip flexed knee (sprint or shoot).
In these two mechanisms, there is a brutal hyperflexion of the hip associated with hyperextension of the knee, causing a violent eccentric contraction of the hamstrings. This is a maximum stretching effect tendons. No direct trauma to the ischial tuberosity were reported.
The sporting gesture was the largest forced deviation (rugby, fencing: slot), a large acceleration, sprint (rugby, skeleton), the shoot into space (football), a forward fall, foot fixed to the ground (rugby, fall cycling, volleyball).
Finally there were two domestic accidents, one out of his car, the other coming out of a lift, the patient slipped by making a forced large gap (break diagnostics makes 3 months in an obese patient not sports).
All patients described the same symptoms involving a violent pain in the buttock (stabbing printing) followed by leg weakness with possible support. Clinical examination revealed a large posterior hematoma and palpation of a vacuum the ischial tuberosity. (Photo 1)

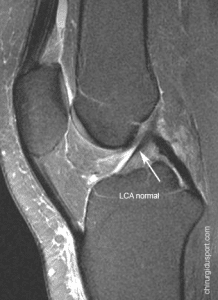
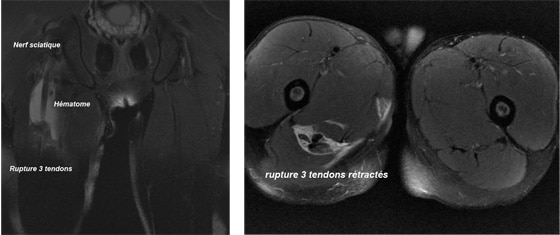
An MRI performed in emergency, for the majority of patients within a period of 4.3 days (1-9 days) confirmed Out of diagnosis (Fig. 1 and 2).
In 2 cases of old fracture, MRI was belatedly sought. For one the severity of the injury was initially underestimated due to a rapid recovery but partial. In either case, the initial diagnosis was asked lumbosciatica despite normal spine examinations Diagnosis of breaking old hamstring was finally placed in the 3rd month by an MRI of the upper thigh with the presence of a scar tissue sheathing sciatica.
Surgical indication:
In case of complete avulsion, the risk is medium-term to see established a major muscle weakness hamstring We donc.réaliser surgical rehabilitation for all patients.
The risk of neurological sequelae of sciatica is described, as was the case for one of the patients in our series.
This is a difficult procedure and especially if it is late.
All patients were operated by two senior surgeons within an average of 10.2 days (5-16) and 3 months for late case. The surgical technique was the same for all patients. Under general anesthesia or spinal anesthesia, the patient is installed in the prone position, the hip slightly flexed 20 ° to support the knee in 90 ° flexion on a knee bar (Fig. 3).

This installation can relax the hamstrings. A short vertical incision of 5 to 8 cm is made in the gluteal fold and plumb with the ischial tuberosity (Fig. 4).
After opening the superficial fascia, we can find the stump of the three tendons severed and retracted (Fig. 5), with deep the sciatic nerve is identified. Early in our experience we realized neurolysis and careful dissection of the sciatic nerve. Subsequently, a simple identification of the sciatic nerve was sufficient for an intervention safely. However, for the former case with sciatica, we achieved a wide release of the sciatic nerve which was adherent to the tendon stump hamstring.
The identification of the ischial tuberosity is difficult because the ischium is hidden under the buttocks. However, after proper exposure, there was conducted a transosseous reintegration of all three tendons by metal anchors and son nonabsorbable SuperAnchor MITEK® GII ™, for the first case 13, was used an average of 3.3 anchors (3 to 4) per patient (Fig. 6, 7). The last 2 cases were treated with absorbable anchors LUPINE ™ Loop Anchor System at MITEK®. The use of “Lupine guide chuck” facilitates the surgical procedure by protecting tissues during the installation of the anchor.
A simple leg splint immobilized the knee flexed at 30 ° for 4-5 days after surgery. Then it was replaced by an articulated thermoplastic toggle ridge on measurement, permitting free knee flexion but a limited extension at 30 °. This was worn for 45 days after surgery (Fig. 8). Partial support was authorized emblem.
Functional rehabilitation was quickly started by an isometric work hamstring muscles for 6 weeks and then relayed by active work. All patients were monitored regularly for the first 6 months and they were reviewed for the study. We analyzed the clinical results (pain, muscle weakness, patient satisfaction, return to sport), isokinetic results (Biodex test) and imaging results (MRI control after 6 months).
Results:
Twelve patients had a total rupture of the three tendons, with a shrinkage measured at 6.2 cm (5 to 10) average, one had more muscle lesion body of the semi-membranous. Three patients had a partial tear of the hamstring: 2 cases had a complete rupture of the semitendinosus and semimembranosus tendon along with partially ruptured biceps, a case had semitendinosus intact other tendons severed.
There were 14 men and women (Table 1). At last follow of 36.6 months (5-76), 94% of patients were satisfied. They had no pain or muscle weakness. One patient complained of a gene at the ischium in prolonged sitting on hard surface. One patient was reoperated 6 years after the first surgery, he had pain in the buttocks on a migrated anchor.
They had resumed their sports activities at the same level to the 5th postoperative month (4.2 to 7.3). Isokinetic test was performed between the 7th and the 12th month, and 7 patients showed an average deficit below 8% (68-107%). Finally MRI control, performed after 6 months has shown a very good healing of tendons 3, with normal muscle signal.
We had two complications: a migration anchor (1 of 4) requiring reoperation late but no effect on the healing of tendons and a superficial burn of the scrotum (the iodized alcohol).
Discussion:
Muscular trauma in the posterior region of the thigh are very common in athletes. It is, in most cases, simple strains hamstring muscles. contact sports, running and jumping are the most commonly involved [1-6]. Rugby is the sport most often involved in this type of injury. In the literature, the rate of injuries hamstring ranges from 18 to 23% of all injuries in rugby [1,2,5,7]. Football is also responsible for a large number of muscle injuries. Depending on the series from 12 to 16% of football injuries cause muscle damage hamstring [1,5,7]
In 2001, in a prospective study, Verrall [5] studied two Australian rugby clubs in a league season 1. He found 30% of trauma to the posterior region of the thigh 23% of muscle injuries Hamstring . He highlighted the risk factors for this type of injury; age over 24 years, black ethnicity, breakdown history.
Brooks in 2005 [1] has the same rate of hamstring injuries by 18%, after studying 11 English rugby clubs over 2 seasons. The results of Gabbe [7] injuries are more frequent during competitions (77%) and accelerated phase.
By cons, lesions hamstrings are less common football (12%) [1,4], while the risk factors are the same: age greater than 23 years, black players, history of breakdown. [4] Injuries occur more often during competitions and at the end of half time. [6]
Functional treatment of these partial lesions myotendinous junction gives good results. Heiser [8] reviewed 46 football players after partial muscle damage hamstring, recovery was on average 2 weeks followed by a rapid return to the field.
In contrast, total breaks hamstring tendons are very rare and the diagnosis is not always immediate. There is often a significant delay between trauma and surgery. Yet the clinic is simple and well described by Ishikawa [9]; it is a violent pain in the buttock, (stabbing printing) followed by leg weakness. Physical examination showed a large posterior hematoma and palpation of a vacuum the ischial tuberosity. The traumatic mechanism combining classic acute hyperflexion of the hip and knee hyperextension with a violent eccentric contraction of the hamstrings. Sallay [14] has described this eccentric contraction mechanism with maximum effect of stretching muscles. In case of total rupture is suspected, an MRI should be performed urgently in order to confirm the diagnosis of rupture. In case of complete rupture of the hamstring urgent specialist advice is necessary because early surgery is easy and effective.
Woods [6] in 2004, only 3 cases of ruptures total of 95 injuries hamstring after following 2376 professional football players for 2 seasons. This rare condition is why today there is no consensus on the treatment of these lesions. The review of literature gives us little article on this subject [9-12,15,16].
The first publications date back to the 90s Ishikawa [9] in 1988 surgically treated two cases, one in emergency (5th day) and the other at a distance (at 2 months) with satisfactory results. Blasier and Morawa [10] in 1990, get very good results with a decline of 7 years after surgical repair performed emergency in a patient suffered a skiing accident, he had a total rupture of tendons 3. Orava and Kujala [11] recommend surgical repair in emergency cases of complete rupture of the hamstring tendons.
In 1998, Cross [12] reported good results in 9 patients operated late after injury (average 36 months) and recommends a strict post operative immobilization, knee 90 ° to 8 weeks. Unlike recent studies that advocate a short period of immobilization to allow the formation of granulation tissue, early mobilization and muscle strengthening are necessary to improve the strength and endurance of the muscle. [13] In our study patients are immobilized for a short time after surgery and began mobilization and early rehabilitation muscle to prevent muscle atrophy.
However, as demonstrated Sallay. [14] functional treatment of these fractures total gives bad results, convalescence is long 3 to 18 months with a limitation or an inability to resume normal sporting activity. Patients complain of pain in the buttock and thigh, ischial pain prolonged sitting, cramps and low leg sensation to effort. The risk of secondary sciatica is important. Isokinetic test shows an average deficit of 61% of hamstrings and quadriceps of 23%. [14]
Our series, like its predecessors, confirms the good results after surgery. The surgical technique using metal anchors and son nonabsorbable SuperAnchor ™ MITEK® GII, simplifies the gesture with a strong trans-rehabilitation without bone tunnel. The recent use of resorbable LUPINE ™ Loop System Anchor anchors in MITEK®, with use of “Lupine guide mandrel” has facilitated the surgical protecting tissues during the installation of the anchor. Immobilization can thus be mild and of short duration with immediate rehabilitation, and improves clinical outcomes. Our sportsmen patients (13 patients out of 15) have resumed their activity in a short time (5 months) and at the same level, Klingele [16] in his series gets the same results with a recovery in the 6th month (12 of 15 patients).
Conclusion:
The complete and proximal hamstring rupture of the sport is a rare but serious injury. Our study, like previous ones, shows that early diagnosis and surgical treatment of these total ruptures can recover a normal functional state with a rapid resumption of high-level sport. Only a short postoperative immobilization is necessary.
We must abandon the functional treatment gives poor results.
In all cases, an MRI should be performed urgently in order to confirm the diagnosis of total rupture of the hamstring tendons, assess the extent of damage, and ask the surgical indication.
References:
[1] Brooks JH, Fuller CW, Kemp SP, Reddin DB. Epidemiology of injuries in English
professional rugby union: part 2 training Injuries. Br J Sports Med. 2005 Oct;39(10):767-75.
[2] Hagel B. Hamstring injuries in Australien Football. Clin J Sport med. 2005 sep;15(5):400
[3] Pertersen J, P Hölmich : Evidence based prevention of hamstring injuries in sport. Br J Sports Med 2005; 39:319-323;
[4] Hägglung M, Walden M, Ekstrand J. Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med 2006;40: 767-772
[5] Verrall GM, Slavotinek JP, Barnes PG, Fon GT, Spriggins AJ. Clinical risk factors for hamstring muscle strain injury: a prospective study with correlation of injury by magnetic resonance imaging. Br J Sports Med 2001; Dec;35(6):435-9
[6] Woods C, Hawkins RD, Maltby S, Hulse M, Thomas A, Hodson A; Football Association Medical Research Programme. The Football Association Medical Research Programme: an audit of injuries in professional football–analysis of hamstring injuries. Br J Sports Med. 2004; Feb;38(1):36-41.
[7] Gabbe BJ, Finch CF, Bennell KL, Wajswelner H. Risk factors for hamstring injuries in community level Australian football.2005; Br J Sports Med 39:106-110
[8] Heiser TM, Weber J, Sullivan G, et al: Prophylaxis and management of hamstring muscle injuris in intercollegiate football players. Am J Sports Med 1984; 12: 368-370
[9] Ishikawa K. Kai K, Mizuta H. Avulsion of the hamstring muscles from the ischial tuberosity. A report of two cases. Clin Orthop 1988; 232:153-155
[10] Blasier RB, Morawa LG, Complete rupture of the hamstring origin from a water skiing injury. Am J Sport Med 1990; 18:435-437
[11] Orava S, Kujala UM. Rupture of the ischial origin of the hamstring muscles. Am J Sports Med 1995; Nov-Dec; 23(6):702-5.
[12] Cross MJ, Vandersluis R, Wood D, Banff M. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med 1998; Nov-Dec; 26(6):785-8.
[13] Kujala UM, Orava S, Jarviven M. Hamstring injuries. Current trends in treatment and prevention. Sports Med 1997; 23:397-404
[14] Sallay PL, Friedman RL, Coogan PG: Hamstring muscle injuries among water skiers. Functional outcome and prevention. Am J Sports Med 1996;24:130-136
[15] Chakravarthy J, Ramisetty N, Pimpalnerkar A, Mohtadi N. Surgical repair of complete proximal hamstring tendon ruptures in water skiers and bull riders: a report of four cases and review of the literature. Br J Sports Med. Aug; 2005;39(8):569-72
[16] Klingele KE, Sallay PI. Surgical repair of complete proximal hamstring tendon rupture. Am J Sports Med. 2002; Sep-Oct;30(5):742-7
Doctor Nicolas LEFEVRE, Doctor Serge HERMAN, Doctor Yoann BOHU. – 12 janvier 2011.